1 Beck CS, Leighninger DS. Scientific basis for the surgical treatment of coronary artery disease. J Am Med Assoc. 1955;159(13):1264–71. doi:https://doi.org/10.1001/jama.1955.02960300008003.
2 Feigl EO. The paradox of adrenergic coronary vasoconstriction. Circulation. 1987;76(4):737–45. doi:https://doi.org/10.1161/01.CIR.76.4.737.
3 Crea F, Galassi AR, Carlos Kaski J, Pupita G, El Tamimi H, Davies GJ, et al. Effect of theophylline on exercise-induced myocardial ischaemia. Lancet. 1989;333(8640):683–6. doi:https://doi.org/10.1016/S0140-6736(89)92204-6.
4 Mannheimer C, Camici P, Chester MR, Collins A, DeJongste M, Eliasson T, et al. The problem of chronic refractory angina; report from the ESC Joint Study Group on the Treatment of Refractory Angina. Eur Heart J. 2002;23(5):355–70. doi:https://doi.org/10.1053/euhj.2001.2706.
5 Mukherjee D, Comella K, Bhatt DL, Roe MT, Patel V, Ellis SG. Clinical outcome of a cohort of patients eligible for therapeutic angiogenesis or transmyocardial revascularization. Am Heart J. 2001;142(1):72–4. doi:https://doi.org/10.1067/mhj.2001.115786.
6 Brorsson B, Bernstein SJ, Brook RH, Werkö L. Quality of life of patients with chronic stable angina before and four years after coronary revascularisation compared with a normal population. Heart. 2002;87(2):140–5. doi:https://doi.org/10.1136/heart.87.2.140.
7 Williams B, Menon M, Satran D, Hayward D, Hodges JS, Burke MN, et al. Patients with coronary artery disease not amenable to traditional revascularization: prevalence and 3-year mortality. Catheter Cardiovasc Interv. 2010;75(6):886–91.
8 Henry TD, Satran D, Hodges JS, Johnson RK, Poulose AK, Campbell AR, et al. Long-term survival in patients with refractory angina. Eur Heart J. 2013;34(34):2683–8. doi:https://doi.org/10.1093/eurheartj/eht165.
9 Lenzen M, Scholte op Reimer W, Norekvål TM, De Geest S, Fridlund B, Heikkilä J, et al. Pharmacological treatment and perceived health status during 1-year follow up in patients diagnosed with coronary artery disease, but ineligible for revascularization. Results from the Euro Heart Survey on Coronary Revascularization. Eur J Cardiovasc Nurs. 2006;5(2):115–21. doi:https://doi.org/10.1016/j.ejcnurse.2006.01.003.
10 Chaitman BR, Skettino SL, Parker JO, Hanley P, Meluzin J, Kuch J, et al.; MARISA Investigators. Anti-ischemic effects and long-term survival during ranolazine monotherapy in patients with chronic severe angina. J Am Coll Cardiol. 2004;43(8):1375–82. doi:https://doi.org/10.1016/j.jacc.2003.11.045.
11 Chaitman BR, Pepine CJ, Parker JO, Skopal J, Chumakova G, Kuch J, et al., Combination Assessment of Ranolazine In Stable Angina (CARISA) Investigators. Effects of ranolazine with atenolol, amlodipine, or diltiazem on exercise tolerance and angina frequency in patients with severe chronic angina: a randomized controlled trial. JAMA. 2004;291(3):309–16. doi:https://doi.org/10.1001/jama.291.3.309.
12 Kosiborod M, Arnold SV, Spertus JA, McGuire DK, Li Y, Yue P, et al. Evaluation of ranolazine in patients with type 2 diabetes mellitus and chronic stable angina: results from the TERISA randomized clinical trial (Type 2 Diabetes Evaluation of Ranolazine in Subjects With Chronic Stable Angina). J Am Coll Cardiol. 2013;61(20):2038–45. doi:https://doi.org/10.1016/j.jacc.2013.02.011.
13 Scirica BM, Morrow DA, Hod H, Murphy SA, Belardinelli L, Hedgepeth CM, et al. Effect of ranolazine, an antianginal agent with novel electrophysiological properties, on the incidence of arrhythmias in patients with non ST-segment elevation acute coronary syndrome: results from the Metabolic Efficiency With Ranolazine for Less Ischemia in Non ST-Elevation Acute Coronary Syndrome Thrombolysis in Myocardial Infarction 36 (MERLIN-TIMI 36) randomized controlled trial. Circulation. 2007;116(15):1647–52. doi:https://doi.org/10.1161/CIRCULATIONAHA.107.724880.
14 Phan TT, Shivu GN, Choudhury A, Abozguia K, Davies C, Naidoo U, et al. Multi-centre experience on the use of perhexiline in chronic heart failure and refractory angina: old drug, new hope. Eur J Heart Fail. 2009;11(9):881–6. doi:https://doi.org/10.1093/eurjhf/hfp106.
15 Vitale C, Spoletini I, Malorni W, Perrone-Filardi P, Volterrani M, Rosano GM. Efficacy of trimetazidine on functional capacity in symptomatic patients with stable exertional angina – the VASCO-angina study. Int J Cardiol. 2013;168(2):1078–81. doi:https://doi.org/10.1016/j.ijcard.2012.11.001.
16 IONA Study Group. Effect of nicorandil on coronary events in patients with stable angina: the Impact Of Nicorandil in Angina (IONA) randomised trial. Lancet. 2002;359(9314):1269–75. doi:https://doi.org/10.1016/S0140-6736(02)08265-X.
17 Tardif JC, Ponikowski P, Kahan T; ASSOCIATE Study Investigators. Efficacy of the I(f) current inhibitor ivabradine in patients with chronic stable angina receiving beta-blocker therapy: a 4-month, randomized, placebo-controlled trial. Eur Heart J. 2009;30(5):540–8. doi:https://doi.org/10.1093/eurheartj/ehn571.
18 Pan X, Bao H, Si Y, Xu C, Chen H, Gao X, et al. Spinal Cord Stimulation for Refractory Angina Pectoris: A Systematic Review and Meta-analysis. Clin J Pain. 2017;33(6):543–51. doi:https://doi.org/10.1097/AJP.0000000000000435.
19 Henry TD, Losordo DW, Traverse JH, Schatz RA, Jolicoeur EM, Schaer GL, et al. Autologous CD34+ cell therapy improves exercise capacity, angina frequency and reduces mortality in no-option refractory angina: a patient-level pooled analysis of randomized double-blinded trials. Eur Heart J. 2018. [Epub ahead of print.] doi:https://doi.org/10.1093/eurheartj/ehx764.
20 Hartikainen J, Hassinen I, Hedman A, Kivelä A, Saraste A, Knuuti J, et al. Adenoviral intramyocardial VEGF-DΔNΔC gene transfer increases myocardial perfusion reserve in refractory angina patients: a phase I/IIa study with 1-year follow-up. Eur Heart J. 2017;38(33):2547–55. doi:https://doi.org/10.1093/eurheartj/ehx352.
21 Mohl W, Glogar DH, Mayr H, Losert U, Sochor H, Pachinger O, et al. Reduction of infarct size induced by pressure-controlled intermittent coronary sinus occlusion. Am J Cardiol. 1984;53(7):923–8. doi:https://doi.org/10.1016/0002-9149(84)90526-5.
22 Syeda B, Schukro C, Heinze G, Modaressi K, Glogar D, Maurer G, et al. The salvage potential of coronary sinus interventions: meta-analysis and pathophysiologic consequences. J Thorac Cardiovasc Surg. 2004;127(6):1703–12. doi:https://doi.org/10.1016/j.jtcvs.2004.01.036.
23 Sato M, Saito T, Mitsugi M, Saitoh S, Niitsuma T, Maehara K, et al. Effects of cardiac contraction and coronary sinus pressure elevation on collateral circulation. Am J Physiol. 1996;271(4 Pt 2):H1433–40.
24 Ido A, Hasebe N, Matsuhashi H, Kikuchi K. Coronary sinus occlusion enhances coronary collateral flow and reduces subendocardial ischemia. Am J Physiol Heart Circ Physiol. 2001;280(3):H1361–7. doi:https://doi.org/10.1152/ajpheart.2001.280.3.H1361.
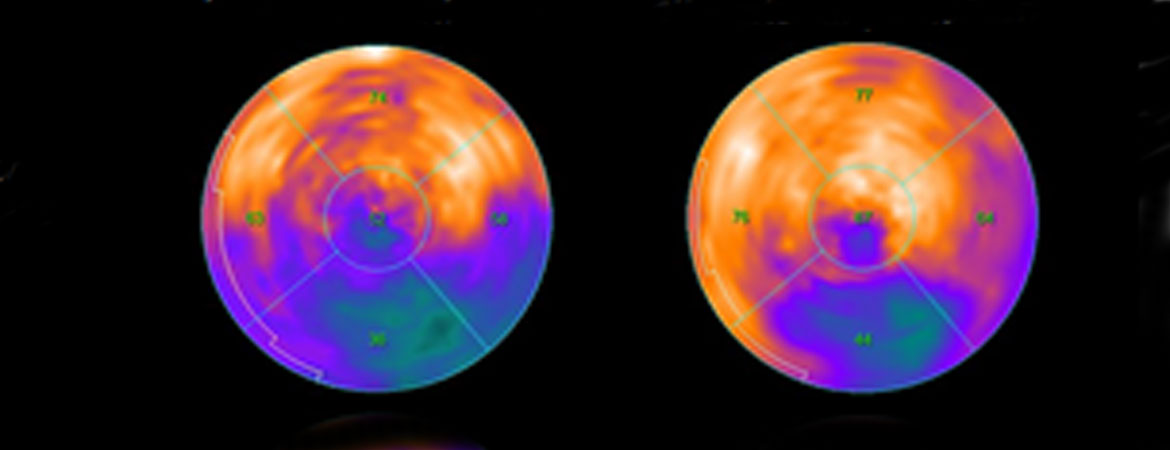
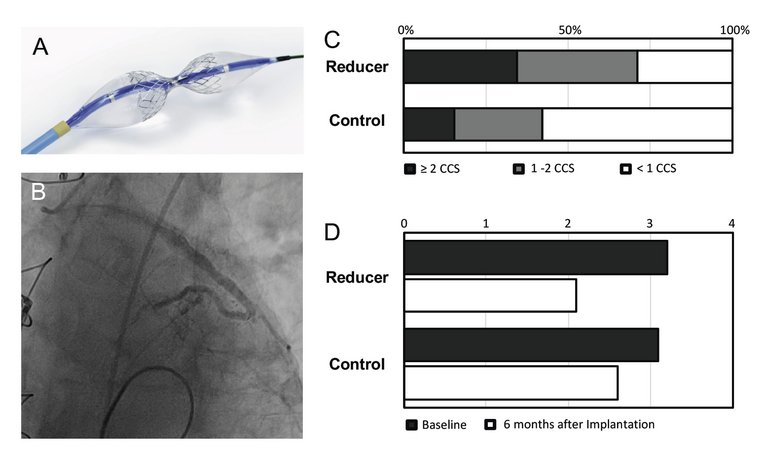
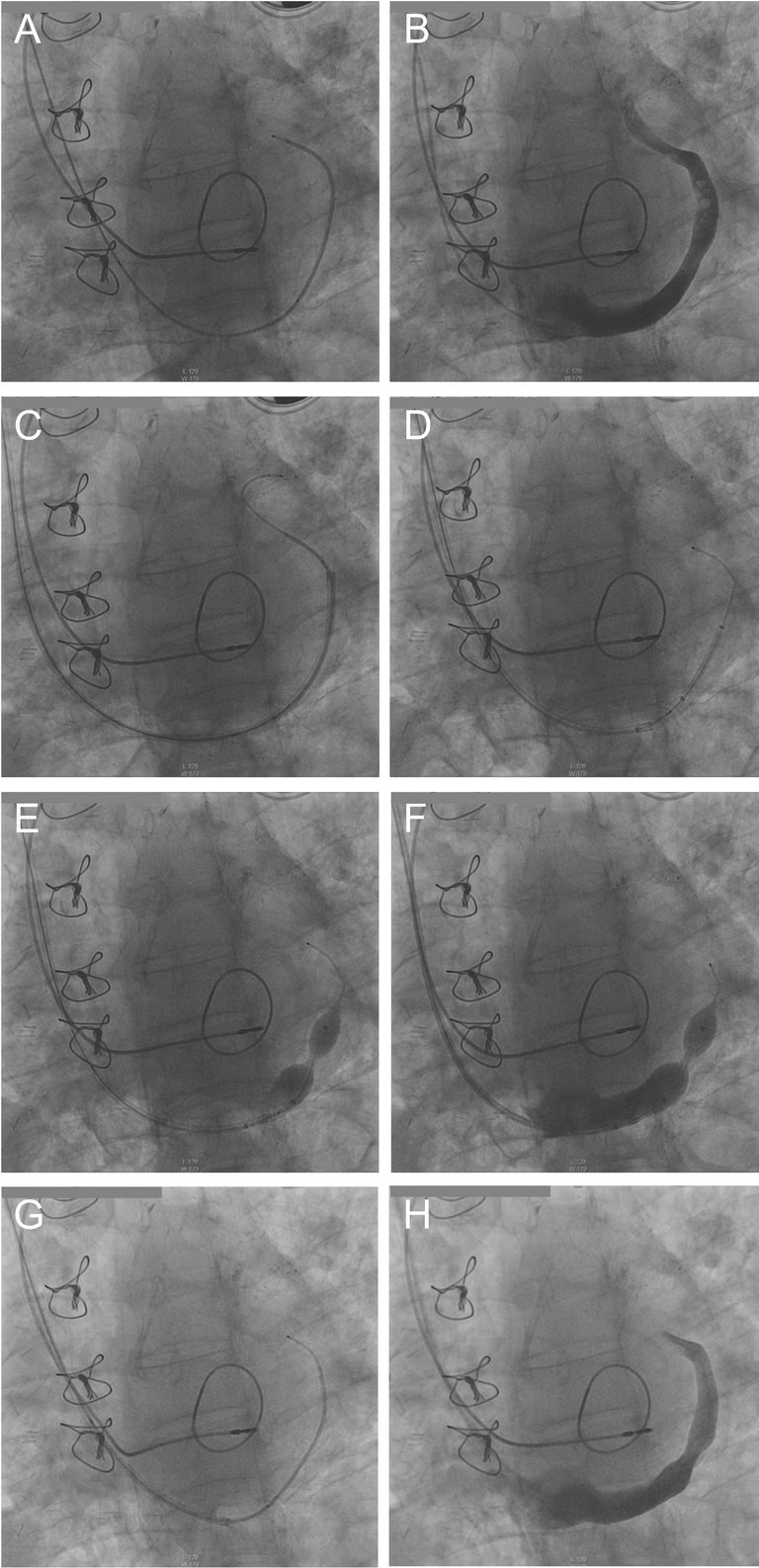
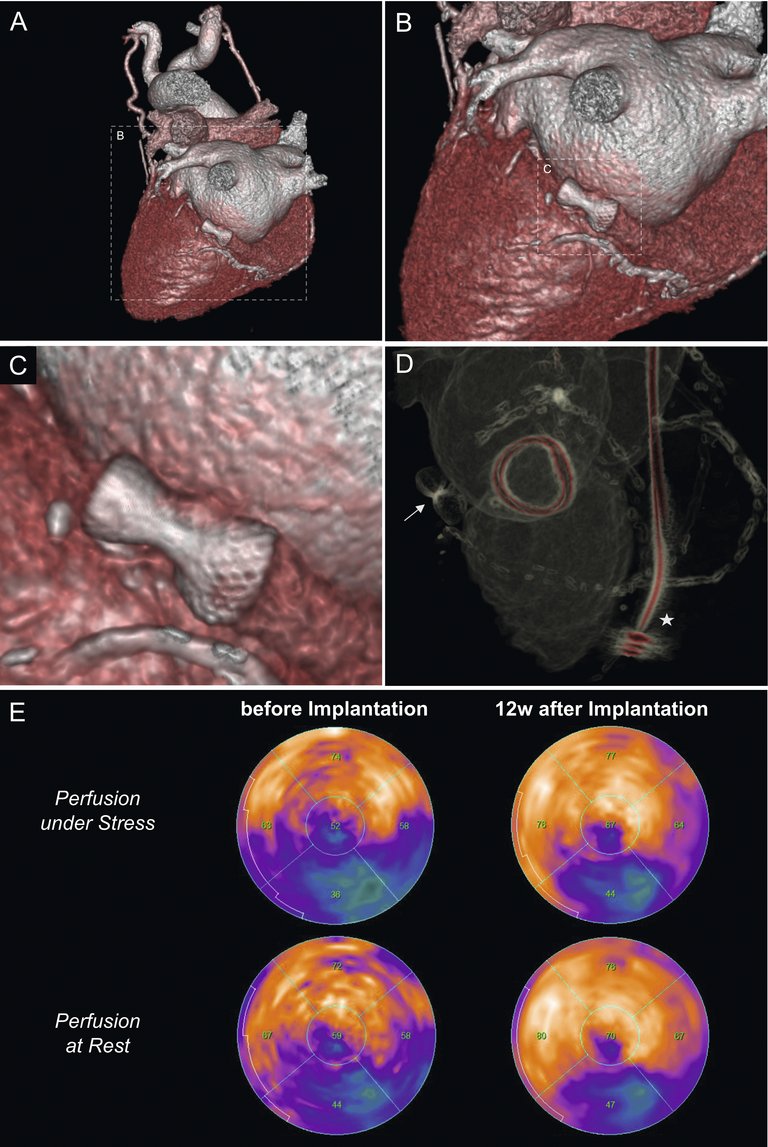
25 Verheye S, Jolicœur EM, Behan MW, Pettersson T, Sainsbury P, Hill J, et al. Efficacy of a device to narrow the coronary sinus in refractory angina. N Engl J Med. 2015;372(6):519–27. doi:https://doi.org/10.1056/NEJMoa1402556.
26 Banai S, Ben Muvhar S, Parikh KH, Medina A, Sievert H, Seth A, et al. Coronary sinus reducer stent for the treatment of chronic refractory angina pectoris: a prospective, open-label, multicenter, safety feasibility first-in-man study. J Am Coll Cardiol. 2007;49(17):1783–9. doi:https://doi.org/10.1016/j.jacc.2007.01.061.
27 Konigstein M, Giannini F, Banai S. The Reducer device in patients with angina pectoris: mechanisms, indications, and perspectives. Eur Heart J. 2017. [Epub ahead of print.] doi:https://doi.org/10.1093/eurheartj/ehx486.